麻省总医院普通外科医生首次将猪肾移植到男性体内 患者情况良好但仍存在许多未知数
【中美创新时报2024年3月22日讯】(记者温友平编译)布莱根妇女医院的外科医生进行了世界上首例肾移植手术七十年后,其姊妹医院马萨诸塞州总医院的医生宣布了一项他们希望同样具有历史意义的成就:将基因工程猪的肾脏移植到人类身上。《波士顿环球报》记者菲利斯·J·弗雷尔(Felice J. Freyer)对此进行下述详细报道。
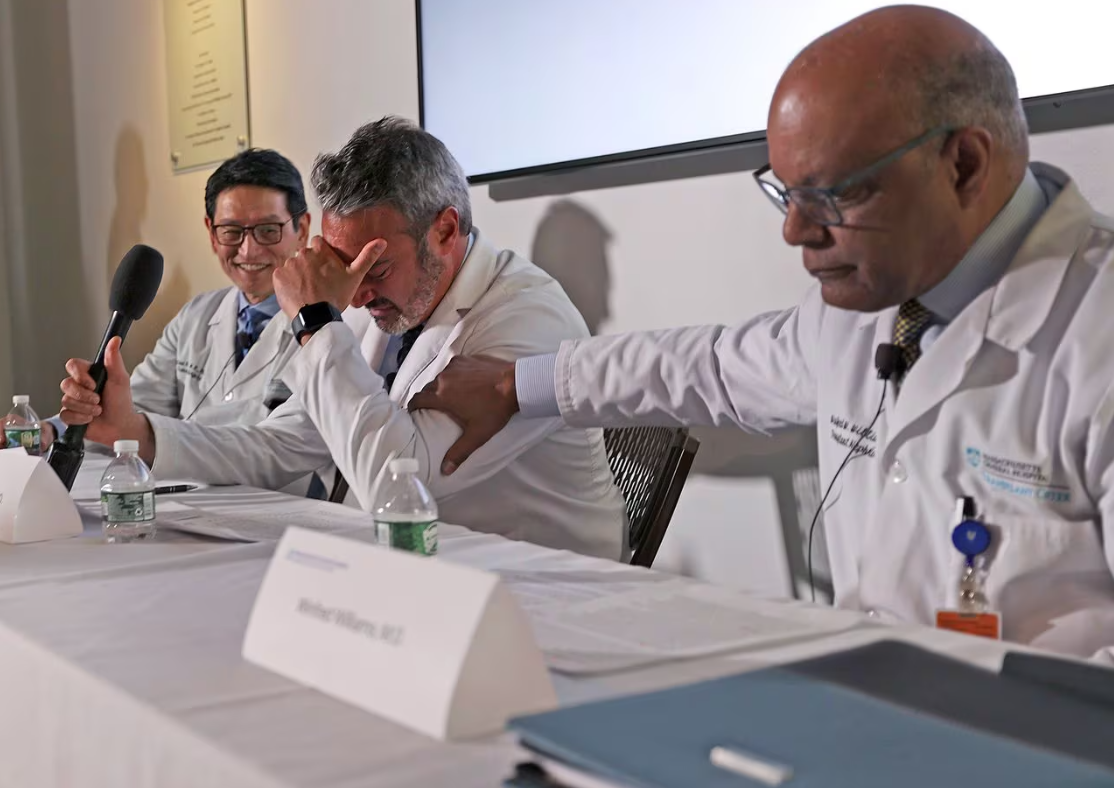
在周四(3月21日)的新闻发布会上,医生们庆祝了这一成就,其中一位医生甚至流泪感谢同事们的贡献。
“每周我们都必须将患者从[移植]等待名单中删除,因为他们病得太重了,”肾移植医学主任莱昂纳多·V·里埃拉(Leonardo V. Riella)博士说。 “今天,我们为许多患者带来了一线希望。”
肾脏接受者是一名 62 岁的韦茅斯男子,在周六进行的四小时手术后情况良好,但只有在未来几周和几个月才能知道移植的器官是否会继续发挥作用。医生将追踪他的肾功能,观察他的身体排斥该器官的迹象,并监测感染情况。
此前的实验已将猪肾移植到脑死亡者和非人类灵长类动物的体内。在过去的两年里,两名男子接受了转基因猪心并存活了长达七周。
这种新的移植手术为稀缺器官(尤其是肾脏)的替代来源带来了希望。据美国卫生资源与服务管理局称,超过 10 万美国人在器官移植等候名单上,每天有 17 人死亡。有色人种尤其难以找到匹配的器官,从而导致了动物器官供应可以纠正的不平等。
“移植研究人员的梦想——圣杯(the Holy Grail)——一直是用猪器官来补充人体器官,解决器官短缺的问题,”麻省总医院移植中心主任乔伦·马德森博士说。
马德森说,人体会在几分钟内排斥普通的猪器官。马萨诸塞州总医院的研究小组经过多年的研究,克服了这一障碍,他们使用了基因经过改变的猪,使其器官不太可能被排斥,以及专门抑制针对猪组织的免疫反应的新药物。尽管如此,被拒绝的可能性仍然是医生们最担心的。

图片:注册护士护理实践专家梅丽莎·马托拉-基亚托斯 (Melissa Mattola-Kiatos) 从盒子里取出猪肾,准备移植,然后外科医生在马萨诸塞州总医院对活人进行世界上首例转基因猪肾移植手术。米歇尔·罗斯/马萨诸塞州总医院
里埃拉说,他的最终目标是透析——用机器净化肾病患者的血液——只能作为临时措施。
美国食品和药物管理局根据其“同情使用”政策批准了移植手术和新的猪特异性免疫抑制剂药物,允许对患有危及生命且几乎没有选择的人进行实验性治疗。
马萨诸塞州普通手术是异种移植研究的又一步,异种移植是将器官或组织从一个物种移植到另一个物种,近年来该研究加速进行。
纽约大学朗格健康中心和阿拉巴马大学伯明翰赫尔辛克医学院的团队将猪肾移植到脑死亡患者体内,而这些患者的亲属也同意进行这项实验;在一例中,肾脏持续了两个月。2022年和2023年,马里兰大学的医生将猪心脏移植给两名男子,但两人均在两个月内死亡。去年,马萨诸塞州总医院的研究人员报告称,经过基因编辑的肾脏在猴子中平均可以保持 176 天的良好功能,而在一只动物中则可以保持两年以上的良好功能。

图片:周六,外科医生在马萨诸塞州综合医院对活人进行了世界上首例转基因猪肾移植手术。米歇尔·罗斯/马萨诸塞州总医院
用于猴子实验的器官来自剑桥的 eGenesis,该公司也为周六的手术提供器官,由著名的哈佛大学遗传学家和生物工程师乔治·丘奇 (George Church) 共同创立。该公司利用CRISPR-cas9基因编辑技术对猪基因组进行了69处调整,消除了会导致人体排斥的特征,并灭活了可能对人类构成威胁的猪病毒。
马萨诸塞州总医院肾脏科副主任温弗雷德·威廉姆斯 (Winfred Williams) 博士表示,马萨诸塞州总医院的患者理查德·“里克”·斯莱曼 (Richard “Rick” Slayman) 是州交通运输部的一名经理,他因糖尿病和高血压而患上肾衰竭。一位认识该患者十多年的移植肾病专家。
经过七年的透析后,斯莱曼于 2018 年接受了捐赠的人类肾脏。一年前,肾脏衰竭,斯莱曼重新接受透析,这对他来说尤其痛苦,因为他的血管多次出现困难。
当斯莱曼有机会获得一种高度实验性的解决方案——猪肾时,他告诉威廉姆斯,他愿意抓住这个机会,因为他的生活是如此悲惨。
威廉姆斯说,斯莱曼是这项实验的良好人选,因为除了肾衰竭和糖尿病之外,他“健康状况相当良好”,并且熟悉移植过程。
周六,麻省总医院 Legorreta 临床移植耐受中心主任 Tatsuo Kawai 博士和移植外科临时主任 Nahel Elias 博士从位于另一个城市的供体猪身上摘除了肾脏。(出于安全原因,马萨诸塞州总医院拒绝透露他们对猪进行手术和饲养猪的设施的位置)。
医生们取出了两个肾脏(其中一个作为备用),将它们放在冰上,然后乘车返回医院,斯莱曼已经在手术台上昏迷不醒。
三名外科医生——埃利亚斯、河合和翔子木村——在两名博士后的协助下进行了手术,他们对移植手术进行了一步一步的描述:他们切开斯莱曼左侧的下腹部,并连接了腹部的血管。将新肾脏移植到他的身上,将其夹紧以避免出血。此时,猪肾躺在斯莱曼的腹部,呈浅米色,其自身的血液已被吸干。然后外科医生取下夹子,斯莱曼的血液流入移植的器官,使它变成鲜艳的粉红色,突然活了过来。
房间里爆发出欢呼声和掌声。猪肾立即开始产生尿液。
“每个人都很高兴,”埃利亚斯说。
随着手术的消息传开,异种移植领域的其他医生也分享了麻省总医院的兴奋之情。
“这是对该领域的推动,”国际异种移植协会主席穆罕默德·M·莫希丁博士在周四接受采访时表示。
在马里兰大学进行了两例猪心脏移植手术的莫希丁表示,他对肾移植抱有“厚望”,这将使该领域更接近下一个目标:涉及更多患者的临床试验。
阿拉巴马大学伯明翰分校移植科主任杰米·洛克博士一直在将猪肾植入脑死亡患者体内。她说她的团队正在与 FDA 就对活人进行类似手术进行谈判。
“如果我们能继续这样做,我们实际上可能能够消除[器官移植]等候名单,并在医疗保健领域首次实现公平,”她说。
当肾病专家威廉姆斯周三检查斯莱曼时,病人正坐在床边。“他看起来就像以前的自己一样,”医生说。“他每天都比前一天进步。”
如果斯莱曼继续健康成长,他可能会在未来几天内出院。威廉姆斯说,他将在第一个月每周回来接受两次测试,并可能在六周内准备好重返工作岗位。
如果猪肾衰竭,斯莱曼将不得不恢复透析。他不会失去在人类肾脏移植名单上的位置。但他已经在名单上两年多了,作为一名黑人,威廉姆斯说斯莱曼可能很难找到肾脏匹配者。
目前,他的医生在保持警惕的同时仍抱有希望。
“人们过去常说异种移植将是未来——而且永远是未来,”外科医生埃利亚斯说。“我们很多人都不会想到我们能在有生之年做到这一点。”
题图:中心肾移植医学主任莱昂纳多·V·里埃拉(Leonardo V. Riella)博士在感谢同事时崩溃了。 Legorreta 临床移植耐受中心主任 Tatsuo Kawai 博士(左)和肾内科副主任 Winfred Williams 博士也在周四的新闻发布会上发表了讲话。DAVID L. RYAN/GLOBE STAFF
附原英文报道:
In a first, Mass. General surgeons transplant a pig kidney into a man
The patient is doing well, but many unknowns remain
By Felice J. Freyer Globe Staff,Updated March 21, 2024
Dr. Leonardo V. Riella, medical director of kidney transplantation, center, broke down as he thanked his colleagues. Dr. Tatsuo Kawai, director of the Legorreta Center for Clinical Transplant Tolerance, left, and Dr. Winfred Williams, associate chief of the Division of Nephrology, also spoke at a news conference on Thursday.DAVID L. RYAN/GLOBE STAFF
Seventy years after surgeons at Brigham & Women’s Hospital performed the world’s first kidney transplant, doctors at its sister hospital, Massachusetts General, announced an accomplishment they hope will prove equally historic: the transplant of a kidney from a genetically engineered pig into a human.
At a news conference Thursday, doctors celebrated the achievement, with one even breaking down in tears as he thanked his colleagues for their contributions.
“Every week we have to remove patients from the [transplant] waiting list because they’ve become too sick,” said Dr. Leonardo V. Riella, medical director for kidney transplantation. “Today we are offering a glimmer of hope to many of these patients.”
The kidney recipient, a 62-year-old Weymouth man, is doing well after the four-hour operation, which took place on Saturday, but only the weeks and months ahead will reveal whether the transplanted organ will continue to work. Doctors will track his kidney function, watch for signs that his body is rejecting the organ, and monitor for infections.
Previous experiments have transplanted pig kidneys in the bodies of brain-dead people and nonhuman primates. In the last two years, two men have received genetically modified pig hearts and lived for up to seven weeks.
This new transplant raises hopes for an alternative source for scarce organs, especially kidneys. More than 100,000 Americans are on waiting lists for organ transplants, and 17 of them die each day, according to the US Health Resources & Services Administration. And people of color have an especially hard time finding matching organs, leading to inequities that a supply of animal organs could correct.
“The dream of transplant researchers — the Holy Grail — has been to use pig organs to supplement the human organs and to solve the problem of the organ shortage,” said Dr. Joren Madsen, director of the MGH Transplant Center.
The human body will reject an ordinary pig organ within minutes, Madsen said. The Mass. General team, after years of research, overcame that obstacle by using a pig whose genes had been altered to make its organs less likely to be rejected, as well as new medications that specifically tamp down the immune response against pig tissue. Still, the prospect of rejection remains the doctors’ prime worry.
Melissa Mattola-Kiatos, an RN nursing practice specialist, removed a pig kidney from its box to prepare for transplantation before surgeons performed the world’s first genetically modified pig kidney transplant into a living human at Massachusetts General Hospital.MICHELLE ROSE/MASSACHUSETTS GENERAL HOSPITAL
Riella said his ultimate goal is that dialysis — in which a kidney patient’s blood is cleansed by machine — will only be used as a temporary measure.
The Food and Drug Administration approved the transplant procedure and the new pig-specific immunosuppressant medications under its “compassionate use” policy allowing experimental treatment for people with life-threatening conditions and few options.
The Mass. General operation is another step in research into xenotransplantation — the transplantation of organs or tissues from one species to another — that has accelerated in recent years.
Teams at NYU Langone Health and the University of Alabama at Birmingham Heersink School of Medicine have transplanted pig kidneys into brain-dead people whose relatives agreed to the experiment; in one case the kidney lasted two months. In 2022 and 2023, doctors at the University of Maryland transplanted pig hearts into two men, but both died within two months. And last year Mass. General researchers reported that gene-edited kidneys functioned well in monkeys for an average of 176 days and in one animal for more than two years.
Surgeons performed the world’s first genetically modified pig kidney transplant into a living human at Massachusetts General Hospital on Saturday.MICHELLE ROSE/MASSACHUSETTS GENERAL HOSPITAL
The pigs whose organs were used in those monkey experiments came from Cambridge-based eGenesis, which also supplied the organ for Saturday’s operation and was cofounded by famed Harvard geneticist and bioengineer George Church. The company used CRISPR-cas9 gene-editing technology to make 69 adjustments to the pig genome, eliminating features that would cause the human body to reject it and inactivating pig viruses that could be a threat to humans.
The Mass. General patient, Richard “Rick” Slayman, a manager with the state Department of Transportation, developed kidney failure as a result of diabetes and hypertension, according to Dr. Winfred Williams, associate chief of the renal division at Mass. General and a transplant nephrologist who has known the patient for more than a decade.
After seven years on dialysis, Slayman received a donated human kidney in 2018. A year ago, the kidney failed and Slayman went back on dialysis, which was especially grueling for him because of repeated difficulties accessing his blood vessels.
When he was offered the chance at a highly experimental solution — a pig’s kidney —Slayman told Williams he was willing to take the chance because his life was so miserable.
Slayman was a good candidate for the experiment because aside from kidney failure and diabetes, he’s in “reasonably good health” and was familiar with the transplant process, Williams said.
On Saturday, Dr. Tatsuo Kawai, director of the Legorreta Center for Clinical Transplant Tolerance at MGH, and Dr. Nahel Elias, interim chief of transplant surgery, removed the kidneys from the donor pig, which was located in another city. (For security reasons, Mass. General declined to release the location of the facilities where they operated on the pig and where the pig was raised).
The doctors removed two kidneys (with one as a backup), put them on ice, and returned by car to the hospital, where Slayman was already unconscious on the operating table.
Three surgeons operated — Elias, Kawai, and Shoko Kimura — assisted by two postdoctoral fellows, and they provided this step-by-step description of the transplant: They cut open Slayman’s lower abdomen on the left side, and attached the blood vessels of the new kidney to his, clamping them closed to avoid bleeding. At that point, the pig kidney lay pale and beige inside Slayman’s abdomen, drained of its own blood. Then the surgeons removed the clamps, and Slayman’s blood flowed into the transplanted organ, turning it a vivid pink, suddenly alive.
The room erupted into cheers and applause. The pig kidney immediately started producing urine.
“Everybody was just elated,” Elias said.
As news of the operation spread, other doctors in the xenotransplantation field shared the excitement evinced at Mass. General.
“This is a boost to the field,” Dr. Muhammad M. Mohiuddin, president of the International Xenotransplantation Association, said in an interview Thursday.
Mohiuddin, who performed the two pig heart transplants at the University of Maryland, said he has “high hopes” for the kidney transplant, which will move the field closer to the next goal: a clinical trial involving a larger number of patients.
Dr. Jayme Locke, director of the Division of Transplantation at the University of Alabama at Birmingham, has been implanting pig kidneys in brain-dead patients. She said her team is in talks with the FDA about performing a similar operation on a living person.
“If we can keep doing this we may actually be able to eliminate the [organ transplant] waiting list and, for the first time in health care, achieve equity,” she said.
When Williams, the nephrologist, checked on Slayman on Wednesday, the patient was sitting on the edge of his bed. “He looks like his old self,” the doctor said. “Every day he’s improving from the day before.”
If the pig kidney fails, Slayman will have to resume dialysis. He won’t lose his place on the transplant list for a human kidney. But he’s been on the list for more than two years already, and as a Black man, Williams said Slayman may have a hard time finding a kidney match.
For now, his doctors are holding onto hope amid their vigilance.
“People used to say that xenotransplantation will be the future — and always the future,” said Elias, the surgeon. “Many of us wouldn’t have thought that we could do it in our lifetime.”

